1
A Shared Understanding of Health Systems Science1
In October and November 2023, the members of the Global Forum on Innovations in Health Professional Education (Appendix B) at the National Academies of Sciences, Engineering, and Medicine held a workshop on Health Systems Science Education. A main objective of the workshop was to explore the importance of training in health systems science (HSS) education to empower learners across the health professions to thrive in, and improve, the systems in which they work, resulting in better care for patients, improved health of populations, and enhanced well-being of health professionals. The workshop was divided into three parts, with an opening session designed to create a shared understanding of HSS, a second session focused on its importance in health professions education, and a third session devoted to exploring the design and implementation of HSS programs in education. Each session included a moderated discussion with the speakers that was captured and shared in the respective chapters of this proceedings. All the sessions for this workshop were planned by a committee in accordance with the Statement of Task (Box 1-1). Workshop agendas can be found in Appendix C.
This Proceedings of a Workshop summarizes the presentations and discussions at the workshop sessions and is divided into four sections.
___________________
1 The planning committee’s (Appendix D) role was limited to planning the workshop. This Proceedings of a Workshop was prepared by independent rapporteurs as a factual account of what occurred at the workshop. The statements, recommendations, and opinions expressed are those of individual presenters and participants and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine. They should not be construed as reflecting any group consensus.
BOX 1-1
Statement of Task
A planning committee of the National Academies of Sciences, Engineering, and Medicine will organize and conduct a public workshop to learn from examples of health systems science education across the learning continuum. Health systems science is the study of how health care is delivered in a way that improves patient care and the ability of patients to navigate the care system. Invited presentations and discussions will involve global audiences in understanding a pathway toward implementing health systems science into curricula by bringing the education and practice sectors together. Invited speakers may present examples and research related to components of health systems science including effective interprofessional education and collaborative practice; aligning education and practice; promoting systems thinking; considering systems competencies; and developing health systems science influencers as change agents for designing resilient, equitable, high-quality health systems while advancing innovation and supporting the well-being of all providers.
Chapter 1 introduces the idea of health systems sciences—what it is, its benefits, and how it might be used within the health professions. Chapter 2 describes the value of HSS across health professions, while Chapter 3 looks at how educators might design, implement, and evaluate training program, and Chapter 4 explores potential strategies for implementing a successful HSS program. The report closes with five appendixes that start with a list of references (Appendix A) and end with a catalog of meeting materials for those seeking additional information on the topic (Appendix E).
UNDERSTANDING HEALTH SYSTEMS SCIENCE
Zohray Talib, California University of Science and Medicine and forum cochair, welcomed in-person and virtual participants to the first session on October 24. “Health system science is a critical area in health professions education,” said Talib. It is no longer sufficient to train health professionals only in patient care; they must learn how to be “stewards of health systems.” This first session, she explained, was aimed at giving all participants a shared understanding of what HSS is and how it fits into the education of health professionals.
Health Systems Science
Raj Ratwani, director of the MedStar Health National Center for Human Factors in Healthcare, opened the workshop by defining a “system”: It is a way to understand a phenomenon through a set of components that interact, follow a set of rules, and have boundaries. A system has dynamic and interactive components that give rise to a unified whole, and the interactions between components are nonlinear. The outcomes are often greater and different than the sum of their parts, he said, which means that looking at individual components alone does not give a broad understanding of the outcomes of a system. Systems science—which is used in complex, high-risk industries, such as defense and aviation—is a systematic process for studying the inputs, components, interactions, and outputs of a system. Applied to the field of health care, HSS is a “foundational framework for the study and understanding of how care is delivered, how health professionals work together to deliver that care, and how the health system can improve patient care and health care delivery.”
Ratwani noted many benefits to an HSS approach. It can improve organizational performance; patient and provider efficiency, experience, and satisfaction; and health outcomes. Looking at the inputs, components, interactions, and outputs of the health care system can give new insights into the organizational processes and performance and lead to improvements across the system. To look at health care through the lens of HSS, it is critical that health professionals from multiple disciplines receive education and training in systems thinking and come together in practice to “get this done.” Ratwani said that bringing together the different perspectives and expertise from various disciplines is instrumental in successfully implementing HSS.
Numerous frameworks have been designed to represent and study health systems; these often emphasize a core component or objective. For example, said Ratwani, the Systems Engineering Initiative for Patient Safety (SEIPS) looks at how people, technology and tools, organizations, environments, and tasks interact and yield patient safety outcomes. He said that each discipline may have its own model of the system, but they usually include the following:
- Core system components, both social and technical;
- Interactions among the components; and
- Important inputs and outputs.
In general, people are linear thinkers, said Ratwani, and this is one of the biggest challenges in incorporating systems thinking into health professions education. People look at individual components of systems
and want to see a clear cause-and-effect relationship between them. For example, conversations around recent railway accidents have focused on identifying a single cause rather than looking at the multiple interacting components that gave rise to them. Linear thinking focuses on disconnected parts, siloes, analysis, and isolation. In contrast, systems thinking looks at interconnectedness, circularity, synthesis, and relationships (see Figure 1-1).
The health care system is complex, said Ratwani, with multiple interacting components that all impact the patient experience; these include providers, electronic health records, devices and equipment, policies, and procedures. To improve outcomes, he added, the interactions and relationships between these components must be acknowledged and addressed. By taking a systems lens and working across disciplines, health professionals and educators can create the necessary advancements.
Kimberly Lomis, vice president of Medical Education Innovations at the American Medical Association (AMA), described how it has been working to train future physicians in systems thinking. In 2013, it launched an initiative to think about the future of medical education with a number of objectives, but a major emphasis was on the need to be a systems thinker and understand one’s role in working with other health professions to obtain optimal patient outcomes. Lomis shared the systems framework developed by AMA (see Figure 1-2), noting that it has been picked up by disciplines beyond medicine. The concepts in the outer rings—including leadership, teaming, and change agency—are areas of competency that can be fostered among learners and are common across all the health professions. She described the competencies involved in systems thinking and teaming to illustrate what they look like in day-to-day work.

SOURCES: Presented by Raj Ratwani on November 1, 2023, at the workshop titled Health Systems Science Education. Illustration created by Emma Segal for 2017 Disruptive Design web article “Tools for Systems Thinkers: The 6 Fundamental Concepts of Systems Thinking.”

SOURCES: Presented by Kimberly Lomis on October 24, 2023, at the pre-workshop titled Health Systems Science Education. Skochelak et al., 2020; Creative Commons 4.0 License; Copyright American Medical Association 2020, all rights reserved.
Systems thinking means the following:
- Thinking/working across multiple domains for patients and families,
- Thinking/planning multiple steps ahead,
- Understanding the impact of actions and inactions,
- Engaging and leveraging the health system to provide quality care, and
- Anticipating system needs/pitfalls.
Teaming includes the competencies of the following:
- Respect for team members and knowing the names and strengths/limits of team;
- Roles, responsibilities, and expertise;
- Gratitude and professional humility;
- Emotional regulation; and
- Effective conflict management.
Lomis emphasized that the patient, family, and community are at the center of the framework but that it is important for the provider to be cognizant of the system surrounding the patient. A systems thinker can “put [their] head up” from the immediate patient interaction to see the system influences surrounding the patient and think broadly about how to leverage the expertise and unique perspectives of other health professions to provide the best care. The AMA, said Lomis, has been promoting HSS as the third pillar of medical education (the first two are basic science and clinical science). To advance HSS as a critically important third pillar, the AMA has developed resources to support those who want to incorporate it into training programs, including a textbook, online modules, faculty-development programs, and an implementation guide.
After implementing the HSS framework and tools, Lomis said that the AMA was curious about whether learners who had been trained in these concepts were using the tools actively. It launched the AMA Health Systems Science Impact Challenge to gather stories and evidence about how students, residents, and fellows were using HSS in their work.
LEARNER PERSPECTIVE
Nicholaus Christian, an addiction medicine fellow in the Yale School of Medicine and a winner of an Impact Challenge award, shared his story of how HSS impacted his learning and career. Christian grew up in Ohio and attended Wright State University Boonshoft School of Medicine in Dayton, where he also pursued a degree in business. The dual-degree program in medicine and business (M.D./M.B.A.) emphasized HSS and encouraged learners to tell their own stories to advocate for change. The opioid crisis had hit his hometown hard, and he had several close friends who had overdosed and died. His personal experiences led him to realize the importance of getting students plugged into projects addressing the crisis. Christian teamed up with a public health organization in the area and worked with different health professional schools to get students involved. Christian began his residency at the Dell Medical School at The University of Texas at Austin that provided training in HSS and had the resources to
complete a project. Christian said that the idea for his project was sparked when he overheard a physician assistant (PA) wonder about why patients with opioid use disorder (OUD) were not given buprenorphine while hospitalized. Buprenorphine is the standard of care and saves people’s lives, yet it was not being offered to those who needed it. He and the PA began brainstorming to develop a plan to implement it.
They spent an afternoon creating a process map to think through the different service lines for patients with OUD in the hospital: They would need to be identified as having OUD at admission, receive buprenorphine while hospitalized, and be connected to an outpatient clinic to continue the treatment at discharge. Out of this mapping process, the Buprenorphine Team (B Team) was launched. It had a tremendous impact on the culture of the hospital and the lives of patients, said Christian. Within the first 2 years, about 200 patients began buprenorphine treatment. About two-thirds followed up at the outpatient clinic, and about one-quarter were still in treatment 6 months after leaving the hospital. The intervention kept patients engaged in their own health care and gave them the opportunity to choose a life with buprenorphine instead of street drugs, said Christian. It has expanded to five hospitals in Texas and treated more than 1,000 patients last year.
Christian shared his thoughts on what made this program work. The “special sauce” was its interdisciplinary nature. The core team included professionals from social work, pharmacy, nursing, and psychiatry; it even had a chaplain to counsel patients. This collaboration set the program up for success, in part because it helped the team be able to think through the entire process, from admissions to the outpatient clinic. Christian’s work led him to a fellowship in addiction medicine at Yale University, a position at VA Health Service, and a new job at the National Institute of Drug Abuse. Christian said he hopes to continue creating better systems for patients with substance-use disorders. He closed by sharing a story of one of the first patients in the B Team program. After leaving the hospital, the patient met with the outpatient clinic provider and was tearful and grateful for the way he had been treated. He was relieved that he had received compassion when he was caught using while in the hospital, but most importantly, he was in “disbelief” that the providers showed how much they cared about him. Christian said that this story reminds him of the importance of keeping the patient as the anchor of the health system and how systems interventions can be transformational for patients’ lives.
SPEECH, LANGUAGE, AND HEARING SCIENCES
Travis Threats, professor and chair of the Department of Speech, Language, and Hearing Sciences at Saint Louis University, began by sharing
details about the scope of practice for speech language pathologists (SLPs). SLPs share responsibility with other professionals for creating a collaborative culture. Collaboration requires joint communication and shared decision making among all members of the team, including the patient and family, to accomplish improved service delivery and functional outcomes for those served. When discussing specific roles of team members, professionals are ethically and legally obligated to determine whether they have the knowledge and skills necessary to perform such services. Collaboration occurs across all SLP practice domains. In addition to direct care responsibilities, Threats said that SLPs manage populations and systems. This includes (a) managing populations to improve overall health and education; (b) improving the experience of those served; and, in some circumstances, (c) reducing the cost of care. SLPs also improve the efficiency and effectiveness of service delivery. SLPs serve in roles designed to meet the demands and expectations of a changing work environment, said Threats.
Next, Threats shared the World Health Organization (WHO) International Classification of Functioning, Disability, and Health (ICF) framework (see Figure 1-3). It is a comprehensive model that considers not just body structure and function (i.e., impairment) but also activities and participation—that is, what people do in their day-to-day lives. In addition,
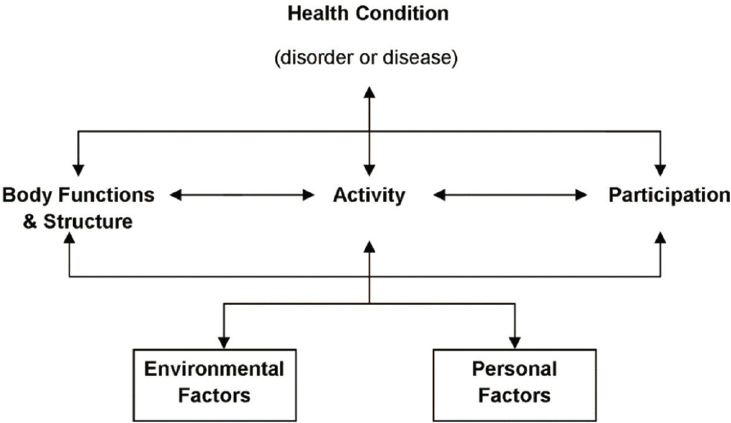
SOURCES: Presented by Travis Threats on October 24, 2023, at the pre-workshop titled Health Systems Science Education. WHO. 2002. “Towards a Common Language for Functioning, Disability and Health: ICF.” CC BY-NC-SA 3.0 IGO license.
it recognizes the interaction between a health condition, environmental factors, and personal factors and how these impact function, activities, and participation. The ICF fits well into HSS in a number of ways, said Threats. First, it represents a comprehensive integration of health condition, real-life functioning, environmental factors, and personal factors; this broad focus echoes HSS’s holistic outlook. Second, it requires a transdisciplinary approach; some of the activity and participation codes2 are so broad that they cannot be addressed without multiple health professionals working together. Third, it focuses on the issues that are important to the individual person, not what the health professional deems important.
Threats shared a hypothetical example of how the ICF framework could be used in an intervention: a 70-year-old woman who had a stroke that left her with mild aphasia and dysarthria, mild oral-stage dysphagia, moderate right arm paresis, and incontinence. The woman has relatively intact cognitive abilities, has been fitted for a hearing aid but rarely uses it, and has dentures that have fit poorly since the stroke. The woman’s husband died 1 year ago, and she has two children, one of whom lives with her and has special needs. She was born in Mexico and is fluent in conversational English but more comfortable talking in Spanish. She worked as a housekeeper in a hotel and now lives solely on her husband’s Social Security check. Using the ICF framework, said Threats, requires starting “at the end” by identifying what is important to her. In this case, an important activity is going to Catholic Mass, often more than once a week. This is classified in the ICF under the activity/participation code for “organized religion.”
To help her get to where she wants to be, multiple health professions could be involved, including SLP, physical therapy, occupational therapy, nutrition, psychology, optometry, nursing, medicine, social work, dentistry, and pastoral care. In multidisciplinary care, each of these professionals should know and respect what the others are doing. However, through the HSS lens, said Threats, each professional must go further and acknowledge that they need one another for the patient to succeed. The work and goals of each professional must be coordinated; for example, improving her eating will require the collaboration of dentistry, SLP, nutrition, and perhaps physical or occupational therapy. In addition to multiple professions working together, patient care requires a careful examination of environmental and personal factors that might serve as facilitators or barriers. For instance, a nursing home patient who is not eating enough might have increasing dementia, but it is also possible that the food is unappetizing. The ICF framework, said Threats, encourages professionals to look at how
___________________
2 ICF activity/participation codes are part of the ICF classification that define activities people might want to engage in such as reading or sports and include qualifiers indicating the level of restriction a person has with engaging in the activity (Threats, 2004).
the environment interacts with the patient rather than seeing everything through the lens of disease.
For this hypothetical patient, the failure to address her personal religious needs could have negative consequences, such as depression, social isolation, medication noncompliance, and physical, cognitive, and mental decline, said Threats. Using the ICF framework to center the patient’s needs and to consider environmental and personal factors allows providers to focus on what matters to the patient and address the systemic factors that may be hindering progress.
SOCIAL WORK
Social work was founded and expanded by people who saw the linkages between health, the economy, the environment, and other factors, said Peter Maramaldi, professor and Social Work Alumni Fund Endowed Chair, School of Social Work, Simmons University. The “mother of medical social work,” Ida Cannon, trained as a nurse and was deeply influenced by the settlement house movement in Chicago around the turn of the 20th century. After finishing her social work studies, Cannon was invited to develop a social service department at Mass General Hospital to work on making medical care more effective. The competencies of social work sit squarely within HSS, said Maramaldi. For example, the National Association of Social Workers describes it as a profession “devoted to helping people function the best they can in their environment.” By addressing the environment that people live in, social workers can help people avoid disease and be healthier.
Social workers operate in a wide variety of environments, including hospitals, universities, and communities, said Maramaldi, and may practice on the micro, meso, or macro levels. For example, at the micro level, they interact with individuals in both private practice and organizations. Those at the meso level might work within groups, possibly as part of an interprofessional health care team at a hospital. Other social workers function at the macro level, leading and establishing social change on a large scale through organizing, advocating for policy change, and as part of the administration. For example, said Maramaldi, two of the architects of the New Deal—Francis Perkins and Harry Hopkins—were both government advisors and social workers. Social workers hold a number of different degrees and may or may not be classified as “social workers,” making it difficult to track the workforce.
Social work’s disciplinary competencies are grounded in ecology, said Maramaldi, taking an ecological perspective of the person in their environment. The Social Ecological Model of Health (see Figure 1-4) shows how that environment is made up of concentric rings that include interpersonal

SOURCES: Presented by Peter Maramaldi on October 24, 2023, at the pre-workshop titled Health Systems Science Education. Illustration adapted from McLeroy et al. (1988) by Tasha Golden.
relationships, communities, policies, and culture. Maramaldi noted that these relationships are not linear and that the environment is constantly dynamic and interacting. This model complements the HSS model presented by Lomis (see Figure 1-1), as it draws attention to the “constellation” of systems and relationships that surround and impact the individual.
Maramaldi emphasized the importance of systems and relationships within social work that place the individual at the core. These initiatives address social needs and the improving health of underserved people and populations, said Maramaldi. They require systems thinking for social workers to understand how individuals and populations are impacted through their work on projects, such as promoting certain congressional
bills, getting billing codes for social work, developing curricular guides, and requiring social work students to study inclusion, equity, and diversity.
PHYSICAL THERAPY
Once you start thinking in a systems science mindset, “it’s really hard to turn it off,” said Catherine Quatman-Yates, associate professor in the Division of Physical Therapy at The Ohio State University School of Health and Rehabilitation Sciences. Quatman-Yates had already earned a Ph.D. in research with a focus on systems science before she began studying physical therapy and entered the health care field. It was an “interesting journey” to go through physical therapy training with a systems lens, when most of her classmates did not begin with that, she said.
The premises and lenses of HSS are part of the physical therapy curriculum, Quatman-Yates noted, but systems-specific terminology and frameworks have only recently been showing up in lectures and activities. Several years ago, the field transitioned to requiring a Ph.D. at the entry level; HSS became a larger part of the physical therapy training curriculum. Quatman-Yates underscored that while HSS terminology and the AMA framework are a newer concept for physical therapy, the field and many of the frameworks for training are based in a systems-thinking lens. Specifically, physical therapists learn how body movement and physical function require multiple body systems and parts to work together. For example, the foot must be positioned in a specific way relative to the head and other body parts for an effective gait. This lens is an inherent part of the profession, she said. There have been a rise in discussions about how the different components and elements of HSS can be more fully integrated into the physical therapy profession. Quatman-Yates added that one of the more prominent ways that systems science has been used in the field is through the idea of learning health systems: As defined by the Institute of Medicine in 2013, this is one in which “science, informatics, incentives, and culture are all aligned for continuous improvement and innovation, with best practices seamlessly embedded in the care process, patients and families active participants in all elements, and new knowledge is captured as an integral by-product of the care experience” (IOM, 2013, p. 136). This idea has been “taken to heart” by many leaders within physical therapy, said Quatman-Yates. For example, one of the leaders of the Learning Health Systems Rehabilitation Research Network is a physical therapist; it offers resources, funding, and support for research on rehabilitation in the health care system.
Quatman-Yates went on to say that many health professionals—including physical therapists—do a good job of cooperating with others to provide quality care to patients. However, what may be even more important is emphasizing a framing of collaboration rather than just cooperation.
Systems need to be set up to create an “immersive space of true collaboration where the intersections are not just acknowledged but actually leveraged in a really powerful way,” she noted. The system is not designed for true collaboration, said Quatman-Yates. Individuals and departments exist in separate bubbles, working on their own independent functions and competing for resources for their own activities and areas of work. Instead of a functioning, dynamic, adaptive machine, health, education, and other sectors are set up as groups of “little bubbles that we hope will participate with one another nicely.” When separate domains function as one and amplify each other’s efforts, that yields real power; the ideal health care system is one in which its outcomes are more than the sum of its parts, she said.
Quatman-Yates closed with a personal anecdote about the power of collaboration to improve patients’ lives. At the start of the COVID-19 pandemic, her father was diagnosed with glioblastoma. Making decisions and facilitating care was enormously challenging, given the realities of the pandemic. Fortunately, she and her sisters all had professional training and experience that helped support his care—one sister is an orthopedic trauma surgeon and another is an intervention specialist. Our health care system should be set up, said Quatman-Yates, so everyone can reap the benefits of having a team of experts cooperating and collaborating to navigate their care.
DISCUSSION
Teaching the Systems Lens
Systems thinking can be difficult for people to grasp, said Lomis, and is not always intuitive. She asked Ratwani about how people can be trained to think in this way. He responded that people tend to be linear thinkers, and this presents a challenge for thinking about how systems work. The job of educators is to meet people where they are and help them take a step back to look at the system as a whole. It can be helpful to walk through the system and remind people that an outcome has multiple contributing factors and that it is usually not possible to determine precisely how and to what extent each component contributes to the outcome. It is also helpful, said Ratwani, to use case studies in demonstrating differences between linear and systems thinking. For example, a case study could show how outcomes might vary dramatically, depending on whether the intervention focused on a specific root cause or used a model of multiple contributing factors.
Christian added that helping people develop a systems lens was critical to creating the B Team. Initially, the intervention met a lot of resistance because people were focused only on what was happening in the hospital. Once providers heard patients’ stories and how their treatment
in the hospital impacted their lives outside of it, they were more able to see the benefit of the program. These stories, said Christian, can be very useful for helping people think more holistically and see how systems impact the personal lives of individuals.
Drawing Boundaries Around Systems
A participant asked Ratwani to clarify how narrow or expansive the definition of a system should be. He noted that, for example, a systems look at diabetes management could include the people, processes, and organizations directly involved in helping someone control their diabetes. However, a more expansive systems view might include influences such as subsidies for corn production, marketing of certain foods, or food deserts in neighborhoods. Ratwani agreed that drawing boundaries around a system is necessary, because otherwise “you can just keep going and going and going.” The boundaries might vary, depending on the point of view of the person using the model. To demonstrate, Ratwani described a practitioner looking to implement interventions to impact diabetes. They might look at the system differently than a policy maker, as each explores different areas for possible interventions. Ratwani encouraged stakeholders to draw boundaries based on things they have or could eventually have direct control over. Because he has no control over corn subsidies, Ratwani says that he would choose not to focus on that particular factor. It can make people “uncomfortable” to draw boundaries, he said, but it is necessary to do that to use the systems lens effectively.
Lomis added that the conversation around boundaries has changed significantly in the last several decades. She recalled that as a medical student, she raised concerns about a child’s home environment and was told that she should only concern herself with “what happens in these four walls.” Although drawing boundaries is necessary, it is also important to push back on boundaries that are too restrictive; even if providers have no direct control over a system factor, she said, they can elevate concerns and point people to other resources.
Coordinating the Team
A participant asked Christian to elaborate on how he ensured that the multiple professionals on the B Team could successfully coordinate and collaborate. Christian responded that he and his colleague decided to not do a lot of planning until they had gathered all the professionals at the table. It was essential to get the input, perspectives, and experiences of multiple disciplines—from the chaplain to social workers to nurses—so they could truly understand how patients moved through the system and how
buprenorphine treatment could best be implemented. Forming the team and having equal representation of different members is critical, he said, so that the plan is not “my idea, it’s our idea.” Maramaldi added that it is not always obvious who should be part of an interprofessional team and that it can be useful to think beyond the usual categories. For example, when at a cancer center, Maramaldi and his colleagues found it difficult to find the time to sit down with patients and really understand their stories and goals. However, the receptionists at the center had a lot of face-to-face time with the patients and were able to get to know them; receptionists were brought into the team as essential members.
Importance of Systems Thinking
Threat emphasized how critical it is to have health professionals who can think through a systems lens. In our system, individuals who have a health situation—whether an overdose or a stroke—are shuffled from the community to the hospital and back again, with little thought of how the environment of the community could help or hinder their recovery. He gave the example of a person who uses drugs who enters care due to an overdose and then is “cut off” from care as soon as the threat of imminent death has abated. They reenter the community and are no longer the responsibility of the hospital, until they overdose again and go back into care. This fragmented system, with little emphasis on the community, is one reason that the United States has poorer health than other nations, despite the abundance of resources, said Threats. Quatman-Yates added that learners can start to build the systems lens early in their training, even before they develop clinical skills. Exposing them to the health care system early can allow them to start to see how the different parts work together—or do not—and the impact these interactions have on patient care. For example, a learner trying to physically navigate a hospital and learning where delays and breakdowns can occur can provide them with useful insight as they pursue their studies in their individual profession.
This page intentionally left blank.
















