Experts discover trigger for deadly motor neurone disease... and the reason may even hit 'healthy' young men
- Has someone you know been affected by MND? Email: [email protected]
- READ MORE: Scientists develop test that may detect dementia nine years earlier
Fresh concerns have been raised over the safety of contact sports after experts uncovered evidence that young rugby players who suffered head injuries were at risk of deadly motor neurone disease.
In two trials, British and US scientists also linked sports-related concussions with dementia and Parkinson-like problems, including tremours and movement difficulty in later life.
The UK experts discovered found players who had been concussed had higher levels of proteins in their blood that may make them more prone to developing the diseases.
The findings come after the death of Leeds Rhinos star Rob Burrow, 41, after a four-and-a-half-year battle with motor neurone disease.
The rare and incurable condition affects the brain and nerves, robbing sufferers of their ability to move, to eat and eventually breathe.

British scientists discovered that players who had had five or more concussions over their careers had higher levels of certain proteins in their blood, linked to conditions including Alzheimer's and even motor neurone disease. It comes as Leeds Rhinos star Rob Burrow (pictured) died last month at the age of just 41 after a four-and-a-half-year battle with MND

Researchers probing the issue — which has been dubbed 'sport's silent scandal' — also found players who had been concussed had lower levels of the protein RBP-4, crucial to help the brain develop and function. Pictured, Rob Burrow in 2013
Dr Karen Hind, UK Rugby Health project lead, honorary fellow at the Wolfson Research Institute for Health and Wellbeing at Durham University and co-author of the first said: 'This is a crucial development in the field.
'We're calling for sustained efforts to define the pathways leading to concussion-induced neurodegenerative diseases.'
Professor Paul Chazot, an expert in the treatment of central nervous system diseases at Durham University and study co-author added: 'This study gives us the beginnings of a biomarker toolbox to periodically monitor the brain health of retired contact sportspeople, particularly those with a history of concussion during their career.
'It will also pave the way for the introduction of the necessary interventions to minimise the development of future neurodegenerative disease.
'We have a range of interventions currently in advanced stages of development.'
In the first study, researchers compared 30 retired male athletes — including both rugby league and rugby union players — who had had five concussions during their careers against 26 retired sportsmen who had no history of concussion.
They found significantly higher levels of the proteins serum t-tau and tau-p181 in the blood among the group who had suffered concussions compared to the control group.
These two proteins are known to play a role in the development of Alzheimer's and motor neurone disease.
Writing in the journal, the International Journal of Molecular Sciences, the scientists added: 'These results could be used as a catalyst to re-evaluate concussion protocols and long-term post-retirement outcomes in sports.'
Jessica Lee, director of research at My Name'5 Doddie Foundation, said: 'These results are preliminary, and the sample size is small, so it's important to approach results with caution.
'However, it will be interesting, with further research, to understand if these biomarkers correlate with disease outcomes.'
In the second study, researchers from Boston University looked at 481 male brain donors with chronic traumatic encephalopathy, a neurodegenerative disease associated with repetitive head impact.
All had played an average of 16 years of contact sports.
Of the volunteers, scientists found almost a quarter (119) displayed Parkinson's-like problems.
A larger proportion of participants with Parkinson's-like symptoms also showed signs of dementia (87.4 per cent) compared to those who had no symptoms (29 per cent).
American football was the most popular sport played among those with Parkinson's like problems.
Around 153,000 people in the UK have Parkinson's, a neurodegenerative condition which causes pain, shaking limbs and difficulties moving.
Every hour two more people are diagnosed and the disease costs the NHS more than £725 million a year.

Dr Karen Hind, UK Rugby Health project lead, honorary fellow at the Wolfson Research Institute for Health and Wellbeing at Durham University and co-author of the first said: 'This is a crucial development in the field.' Pictured, Rob Burrow receiving his MBE in 2022 with wife Lindsey

Scientists hope the discovery could lead to a 'toolkit' to test and monitor these specific blood proteins in players to provide early intervention. Pictured, Rob Burrow being made a CBE by the Prince of Wales in January
Meanwhile, around 944,000 in the UK are thought to be living with dementia, with the figure is thought to be around 7million in the US.
Alzheimer's affects around six in 10 people with dementia.
It is thought to be caused by a build-up of amyloid and tau in the brain, which clump together and from plaques and tangles that make it harder for the brain to work properly.
Eventually, the brain struggles to cope with this damage and dementia symptoms develop.
Memory problems, thinking and reasoning difficulties and language problems are common early symptoms of the condition, which then worsen over time.
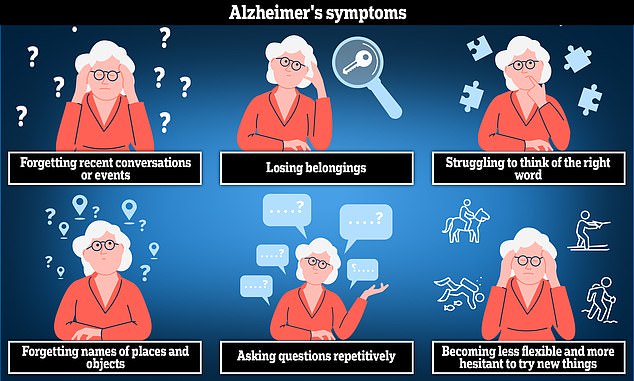
Alzheimer's disease is the most common cause of dementia. The disease can cause anxiety, confusion and short-term memory loss

Knowing the symptoms of Parkinson's can lead to earlier diagnoses and access to treatments that improve patients' quality of life
Dementia are expected to sky-rocket in the coming years, making a cheap screening tool vital to get to grips with the challenge.
Alzheimer's Research UK analysis found 74,261 people died from dementia in 2022 compared with 69,178 a year earlier, making it the country's biggest killer.
Around 5,000 adults in the UK have MND and there is a one in 300 risk of developing the condition over the course of a person's life.
Muscle twitches and a weak grip are among the early signs of MND, along with weakness in the leg or ankle, slurred speech and weight loss.
Some tremors are normal and can be caused by caffeine, stress and age.
There is no cure but doctors can provide treatments to help reduce the impact it has on a person's life.



















































































































































































































































































































































































