Health & Fitness
Tampa Bay Hospitals Sound Alarm With Wave Of Delta Variant Cases
"We were all looking to be out of this pandemic, but we're back in it," said Dr. Peggy Duggan, Tampa General Hospital chief medical officer.
TAMPA, FL — Tampa Bay health care experts are sounding the alarm as the delta variant of the COVID-19 virus sweeps through the area and hospitals struggle to keep up with the increases patient census due to this more virulent strain of the coronavirus.
Already, some hospital groups have suspended elective procedures and surgeries in light of the growing hospital census.
AdventHealth announced Friday that it is postponing elective procedures requiring overnight stays at its hospital in Wesley Chapel starting Monday.
Find out what's happening in Tampawith free, real-time updates from Patch.
No other West Florida Division AdventHealth hospitals are affected at this time.
For now, AdventHealth said it will continue to perform same-day procedures that do not require an overnight stay at the Wesley Chapel hospital.
Find out what's happening in Tampawith free, real-time updates from Patch.
The hospital group said the decision will allow it to plan for an increased need for hospital beds as coronavirus rates continue to surge in Florida due to the introduction of the delta variant of the virus.
AdventHealth noted that more than 90 percent of its patients hospitalized with COVID-19 across the health care group's nationwide system are unvaccinated.
"AdventHealth continues to see a significant increase in COVID-19 cases at its facilities across West Florida and have surpassed our highest peak since the pandemic began in 2020," said AdventHealth in a news release. "We have seen an increase in COVID hospitalizations in AdventHealth hospital locations in Hardee, Highlands, Hillsborough, Marion, Pasco and Pinellas counties."
If cases continue to rise, AdventHealth assures the public that it has sufficient personal protective equipment, ventilators and specialized equipment to quickly and safely convert existing spaces in the hospital into standard patient rooms or critical care rooms for coronavirus patients.
Additionally, starting Monday, AdventHealth Wesley Chapel will begin limiting visitors. Other AdventHealth hospitals in Hillsborough, Pasco and Pinellas counties will begin updating visitation policies as needed beginning later in the week.
On Wednesday, BayCare Health System announced that it will curtail elective procedures requiring overnight stays at hospitals in Hillsborough and Polk counties due to the rising number of patients hospitalized with the coronavirus.
In a news release, BayCare Health said, in the past three weeks, COVID patients in BayCare hospitals have increased more than three-fold.
Hospitals impacted include St. Joseph's, St. Joseph's Children's and St. Joseph's Women's in Tampa; St. Joseph's North in Lutz; St. Joseph's South in Riverview; South Florida Baptist in Plant City; Bartow Regional Medical Center; Winter Haven and Winter Haven Women's.
St. Joseph's, Winter Haven and Winter Haven Women's paused elective procedures Thursday. The other facilities in Hillsborough and Polk counties will pause on Monday.
BayCare hospitals in Pinellas and Pasco counties are not impacted.
"Our priority is always patient safety and being sure we are available to serve our communities' acute health needs," said Glenn Waters, BayCare's chief operating officer. "This move helps us to continue to have capacity to serve those needs."
Tampa General Hospital has not yet announced a similar postponement of elective procedures.
TGH postponed elective surgeries and procedures during the height of the pandemic last year and only resumed them on May 4.
However, the hospital said coronavirus cases at its facilities "have risen dramatically over the past three weeks, more than tripling in number and remaining very volatile."
The hospital noted that 80 percent of the coronavirus patients it is seeing have not been vaccinated.
“It’s critical for people to get vaccinated, especially in this moment,” said Tampa General Chief Medical Officer Dr. Peggy Duggan. “What we’re seeing now is a pandemic of the unvaccinated.”
Duggan said the hospital is seeing younger patients as well. During the initial wave of the disease last year, the median age for patients in Tampa General’s Intensive Care Unit was in the mid-70s. Now it’s 42 years old, she said.
“The risk of the Delta variant is high, and if you’ve had COVID in the past, you can still get this variant – a common misunderstanding people have – and you can give it to each other,” Duggan said. “It’s such a highly contagious disease – about 60 percent more infectious – that right now we’re seeing whole households get the Delta variant, whereas before one or two people could avoid getting infected.”
Over the past year, older people, people with underlying health conditions and health care workers have been more likely to get the vaccine. The higher incidence among younger and healthier people now, Duggan said, is because “they are the last group to get vaccinated and to take it seriously.”
Those who have been fully vaccinated can still become infected, but their symptoms are generally milder and they are less likely to need hospital care, she said.
For those who have not been vaccinated, the risks are sharply heightened amid this highly infectious new strain, which was first identified in December 2020, and rapidly became the dominant strain of the virus in India and Great Britain, Duggan said.
This month Florida made up about 20 percent of new COVID-19 cases in the United States.
“I think humans have a tendency to say, ‘It’s not going to happen to me,’ and when it happens to them it, it can be too late,” said Dr. Seetha Lakshmi, Tampa General’s medical director for the Global Emerging Diseases Institute and assistant professor at the USF Health Morsani College of Medicine.
“There is no need for the human suffering and death that I see today – it is so preventable,” Lakshmi said. "It just breaks my heart. The central message is that even though the vaccine might not prevent you from catching the disease, it will prevent you from seeing us in the ICU and losing your life.”
Some parents may have been reluctant to vaccinate their teenagers after hearing about rare reported cases of myocarditis, an inflammation of the heart, among some teenage boys who received the vaccine. But Lakshmi points to recent data from the Advisory Committee on Immunization Practices that underscores the clear benefit of the vaccine.
In 674 confirmed cases, young males have gotten the condition after the second vaccine dose, but the cases were very mild, no prescription medicine was required (with only Aleve or Advil needed), and no fatalities have resulted.
Meanwhile, more than 11 million young adults ages 18 to 24 have been vaccinated in the US.
“ACIP came out and said, ‘Please get the vaccine and this is the reason why: For every million doses of vaccine given to adolescents we prevent 215 admissions, 71 ICU admissions and two deaths in this age group, compared to 56 cases of mild myocarditis,’ ” Lakshmi said.
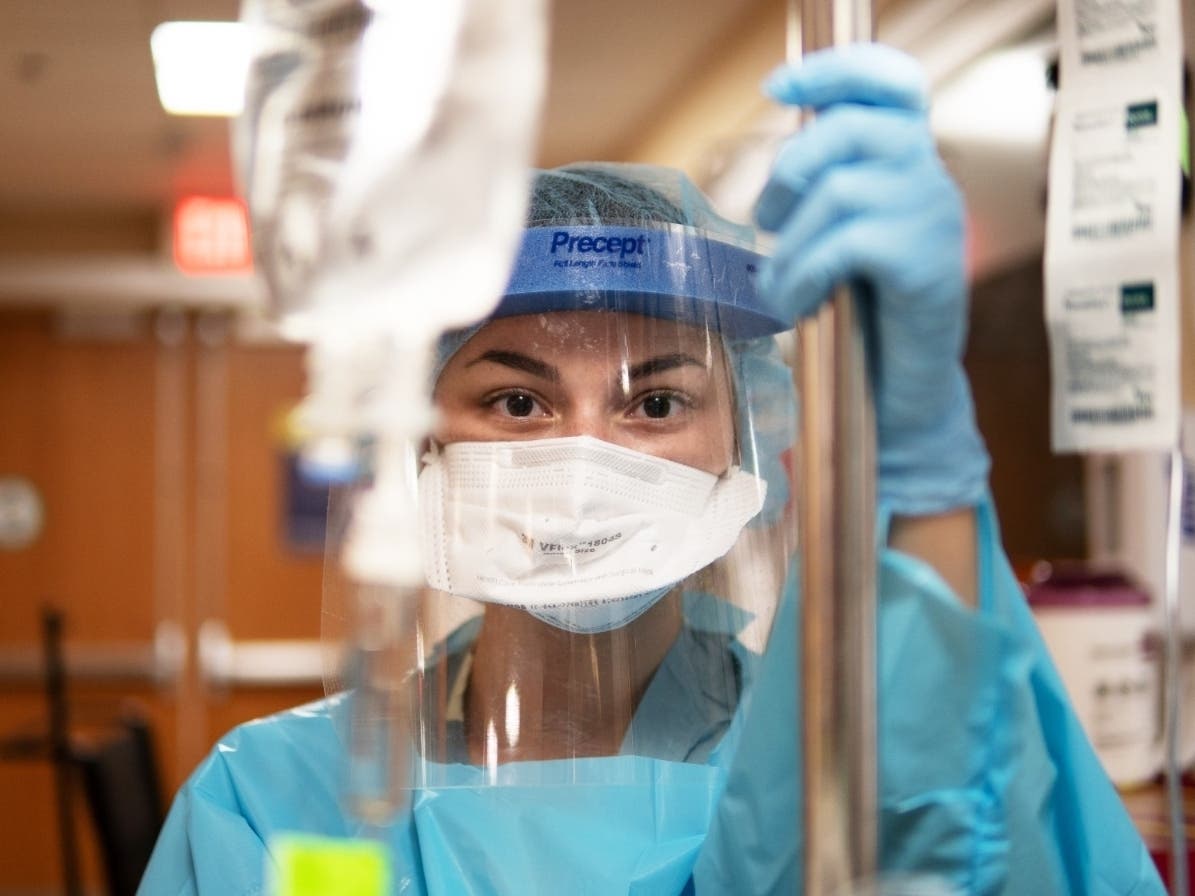
The rise in Delta variant cases has been understandably difficult for some frontline health care workers, who have been thrust back into the physical and emotional whirlwind of caring for COVID patients fighting for their lives.
Now they are faced with a jarring new reality of seeing patients closer to their own ages.
“Our staff is exhausted from the year they’ve been through, and there are some who feel frustrated because this feels avoidable,” Duggan said. “And as a young provider, when you start to look at your patients and they look like you – and it could be you – it does impact you differently. You’re looking at yourself, and it’s tough.”
Both doctors said the best thing residents can do for themselves and their families is to get vaccinated.
“It’s going to protect you, your family and the community,” Duggan said. “It’s really imperative that we all take safety precautions that are common sense. In my own practice, for instance, I’ve limited going out and wear a mask when I go to the grocery store. I may be fine, but I still may pass this virus on to someone else – and that’s the last thing I want to do.
“This doesn’t have to last for a long time. If we can continue to take precautions and move the vaccination rate needle, it will really make a difference. We were all looking to be out of this pandemic, but we’re back in it. So we need to take these steps to get us out of harm’s way," she said.
On Wednesday, the CDC issued a recommendation that all residents wear masks in indoor public spaces including schools.
In Florida, 66 of 67 counties are listed as having "high" levels of community transmission of the coronavirus. Glades County is the only Florida county that's listed as having a "substantial" level of community transmission.
The Centers for Disease Control and Prevention consider a county to have "high" transmission if there have been 100 or more cases of the coronavirus per 100,000 residents or a test positivity rate of 10 percent or higher in the past seven days.
According to the CDC's data tracker, five Florida counties — Duval, Hillsborough, Orange, Miami-Dade and Broward — have had 5,000 or more new cases in the last seven days.
The statewide average is 49 new cases per 100,000 people each day, more than three times the average rate in the United States of about 16 new cases per 100,000 people each day.

See related stories:
Get more local news delivered straight to your inbox. Sign up for free Patch newsletters and alerts.